Brain Cancer
Creating innovative treatments for the deadliest form of brain cancer

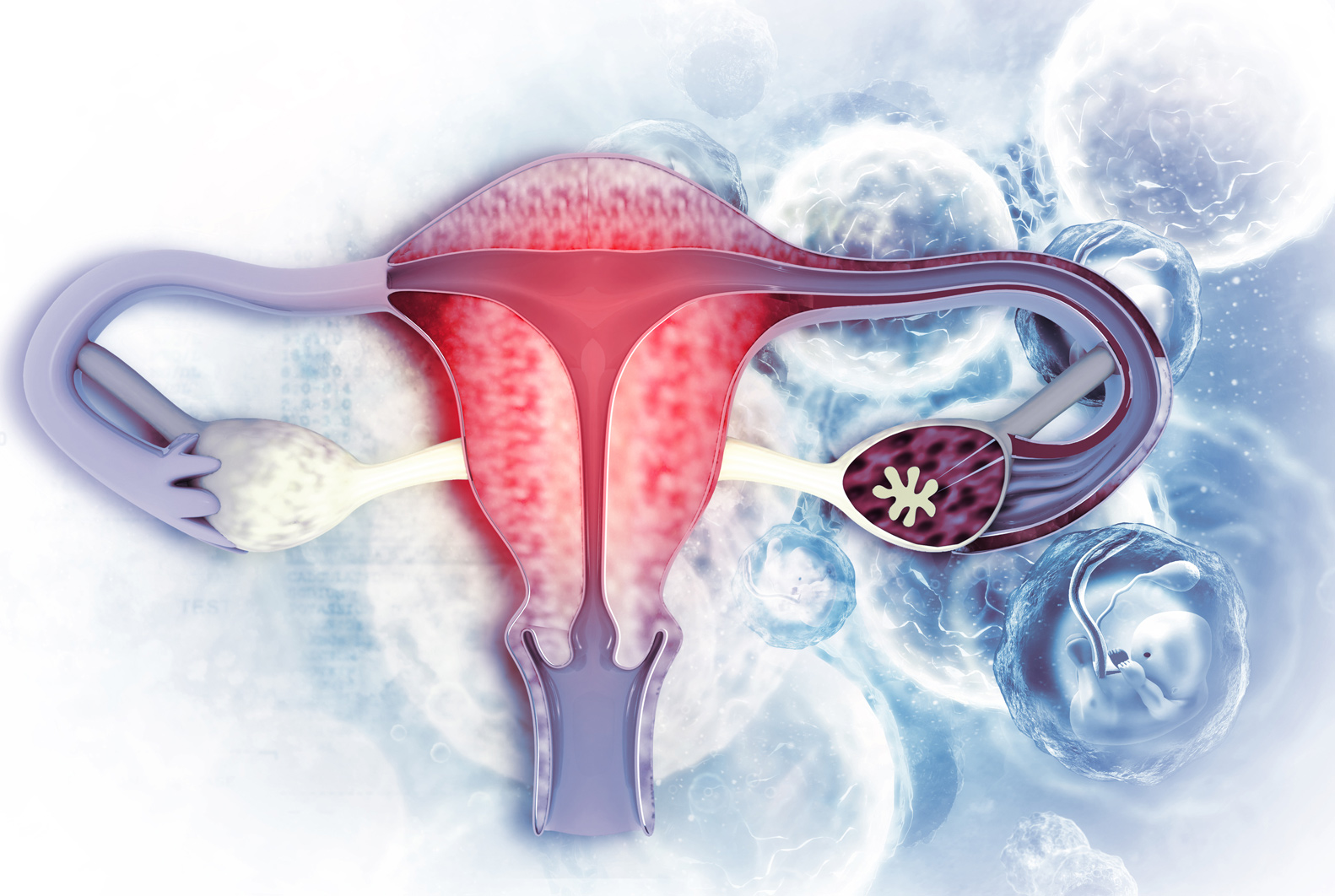
Glioblastoma multiforme (GBM), is the most aggressive form of brain cancer, having an average survival time of 12 to 18 months. Because of the challenges in treating GBM together with very poor survival outcomes, a lot of research continues to be done in this field.
Currently, the first treatment patients receive is surgery, followed by chemotherapy and radiation. The outcome can be improved by enhancing radiation treatment and overcoming resistance to chemotherapy. The multidisciplinary research team at the Institute is approaching these areas by looking at how to improve radiation treatment and how to fight drug resistance.
Diagnostic Magnetic Resonance Imaging (MRI), a non-invasive medical imaging technology used to assess a tumour’s response to treatment is done as a surgical follow-up to see how the tumour is responding to treatment, and whether there is progression or recurrence.
About fifty percent of the time the MRI shows the tumour has increased in size in the first 6 months. For some patients, this progression is a reaction to treatment and not a growth in the tumour. This is called pseudoprogression.
“The challenge is you can’t tell the difference between whether the cancer is progressing or if it is pseudoprogression,” says Dr. Marshall Pitz. “It is important to determine which is which. With our current MRI techniques, we can’t tell.” It is essential to differentiate between the two since treatments for each are vastly different from one another.
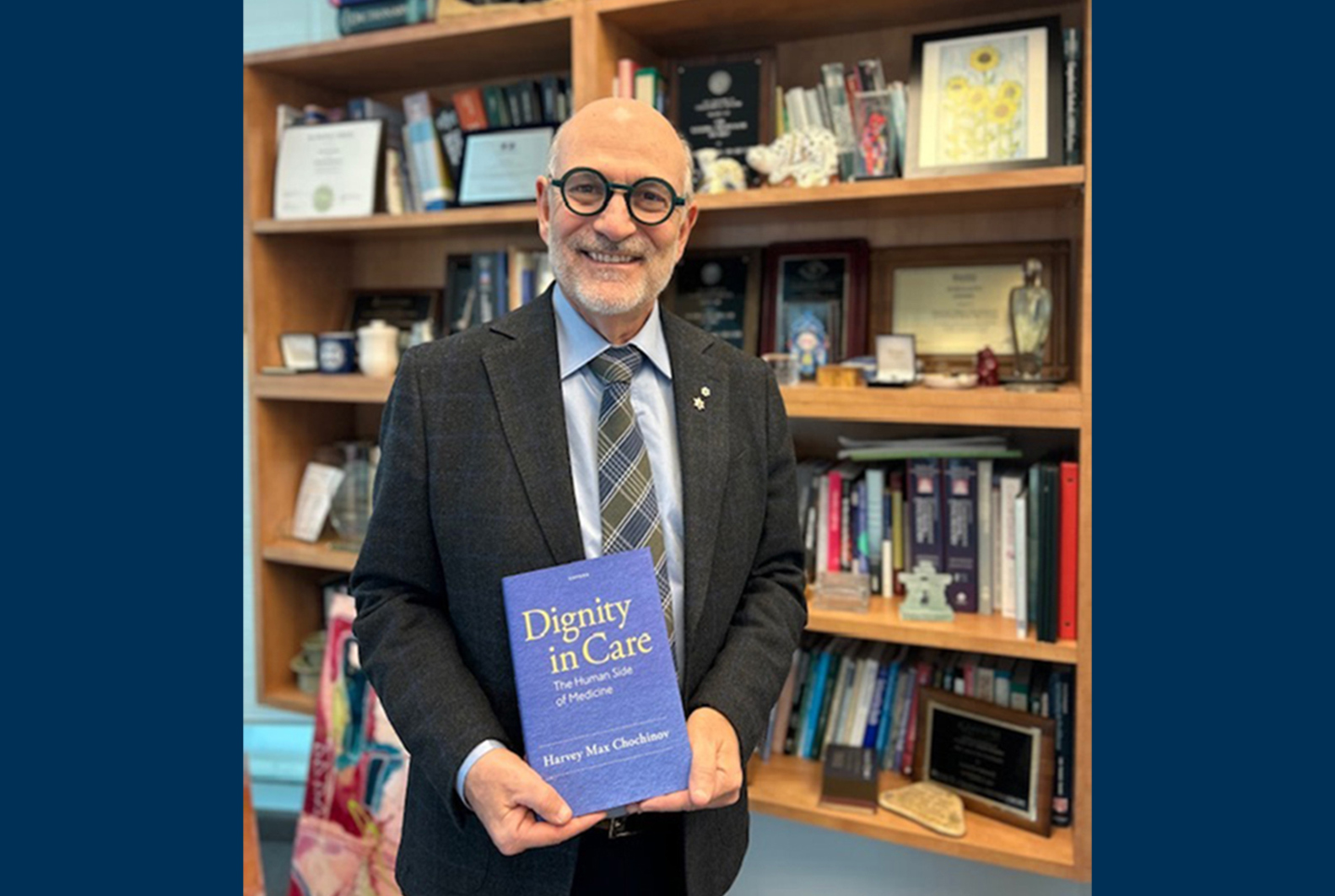
Dr. Pitz
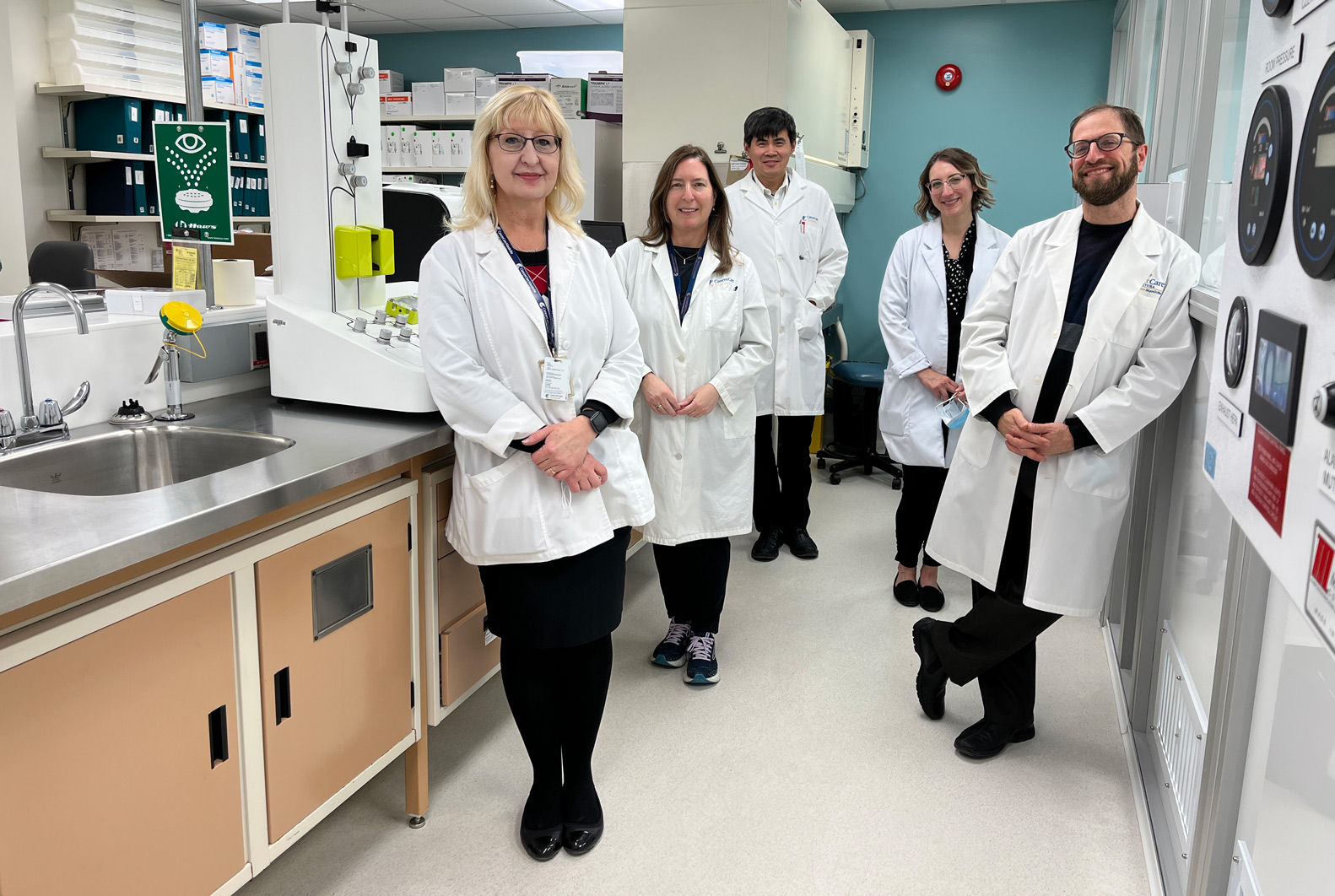
Dr. Pitz, a clinician scientist and medical oncologist who treats patients with brain cancer at CCMB, leads a multidisciplinary team with fellow researchers: Dr. Boyd McCurdy and Dr. Lawrence Ryner, Medical Physicists at CCMB, Dr. Marco Essig, Director of Diagnostic Imaging at Shared Health and Adjunct Scientist at the Institute, as well as Dr. Ahmed Ashraf, Data Scientist in Computer Engineering at the University of Manitoba. The team is studying the use of new advanced MRI sequences to gain additional information about the tumour. This includes identifying pseudoprogression and predicting the location and timing of progression in this disease using artificial intelligence (AI). The team is exploring the ability to modify radiation treatment plans based on the prediction information to see if this will improve the treatment and delay disease recurrence while minimizing treatment to parts of the brain at lower risk.
Dr. Sachin Katyal, a Senior Scientist and brain tumour researcher, is looking at the resistance of the tumour to chemotherapy. Drug resistance is pervasive in GBM disease, resulting in tumour recurrence and leaving GBM patients with few follow-up options. Dr. Katyal is looking at identifying ways tumour cells evade chemotherapeutic drug action and harnessing this knowledge to find ways to resensitize GBM to these drugs. Every cell in our body has an inborn capacity to repair DNA damage caused by the environment, the foods we eat and the drugs we may consume so that our cells survive, thrive, and regenerate. Most chemotherapies are intended to hone in and cause significant DNA damage to tumour cells and overwhelm this DNA repair mechanism; however, tumour cells can develop an ability to ramp up this repair activity and become chemoresistant. Dr. Katyal has identified a specific part of the tumour cell’s DNA repair mechanism that is overactive, and he and his research team and collaborators have identified a new drug that may quell this hyperactive repair activity to allow for chemotherapies to regain their tumour-killing ability.